In the United Sates, around 795,000 people have a stroke each year, but what is a stroke? Understanding what strokes are and risk factors can greatly reduce your risk. If you or a loved one has had a stroke, knowing what to do and what your options are for rehabilitation can greatly improve recovery.
What Is a Stroke?
A stroke is the sudden disruption or loss of the normal blood flow to the brain, resulting in damage to the brain tissue. It affects the arteries of the brain and occurs when blood vessels in the brain burst or are blocked by a clot. This prohibits the affected part of the brain from getting the oxygen and nutrients it needs for nerve cells to function.
Stroke is a non-traumatic type of brain injury. When any kind of brain injury occurs, it can affect your ability to think and move. The part of your brain where stroke occurs will impact how it affects these abilities.
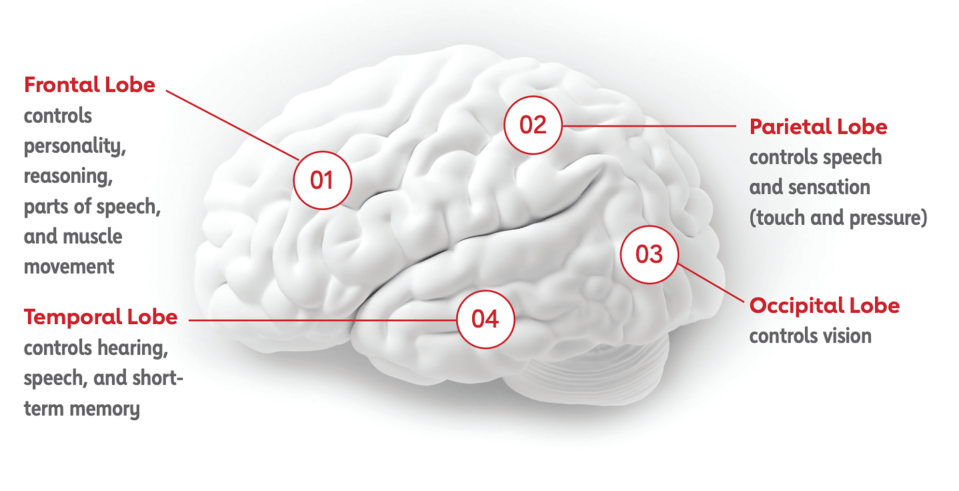
The different areas of the brain control are:
- Frontal lobe: personality, reasoning, parts of speech and muscle movement
- Temporal lobe: hearing, speech and short-term memory
- Parietal lobe: speech and sensation
- Occipital lobe: vision
There are many different types of stroke—some more common than others.
- Ischemic: These strokes occur when the blood flow in the brain, either deep in the interior or in the carotid artery in the neck, is blocked because of a clot that forms in the artery. Ischemic strokes account for more than 80 percent of strokes.
- Hemorrhagic: These strokes account for only 10 percent of all strokes. A hemorrhagic stroke occurs when the walls of an artery in the brain ruptures and blood floods the brain. These are also called a ruptured aneurysm.
What Are the Risk Factors for a Stroke?
There are many risk factors for stroke. Some of them aren’t controllable. Your risk of stroke increases as you age, although they can occur at any time—read Steffany’s story of surviving a stroke at 24.
Your risk also increases if you’ve had a previous stroke. However, there are several strategies for preventing stroke.
- Watch your blood pressure. High blood pressure is the single most important risk factor for stroke, but it is something you can control through medication and lifestyle changes.
- Lower bad cholesterol. Lifestyle changes and medication can keep your LDL, or bad cholesterol, at normal levels.
- Manage diabetes. If you have diabetes, work with your physician to keep your A1C controlled.
- Exercise. Moderate exercise that causes you to break a sweat can also benefit a number of other stroke risk factors.
- Stop smoking. Smoking is a major risk factor for heart disease and stroke.
What Are the Signs and Symptoms of a Stroke? What Should You Do If Someone Is Having One?
A stroke is a medical emergency. The acronym BE FAST can help you identify signs of stroke and know when to call emergency medical services.
- B: Balance—is there a sudden loss or change?
- E: Eyes—is there a change in vision?
- F: Face—does one side of the face droop when smiling?
- A: Arm—does one side drift downward when arms are raised?
- S: Speech—does speech sound slurred?
- T: Time to call 911 if you observe these signs.
If you or someone you know are experiencing any of these symptoms, it’s imperative to seek medical attention immediately. The sooner a stroke is diagnosed, the sooner treatments can be administered.
Diagnosing a Stroke
If you are experiencing symptoms of a stroke, a doctor will make a diagnosis by gathering information on:
- Your medical history
- A physical and neurological exams
- Diagnostics tests such as blood work and radiological tests, such as an CT scan or MRI, may be done
These tests can examine the brain to determine where and what type of stroke occurred to determine the necessary treatments and recovery options.
Common Effects of Stroke
Effects of a stroke vary, and the severity is unique to each stroke survivor.
Physical Impairments
After a stroke, physical impairments may include:
- Weakness in certain limbs or muscles
- Spasticity, or high muscle tone
- Flaccidity, or low muscle tone
- Reduced feeling in a limb, face or abnormal movements
- Problems with balance or coordination
- Apraxia, which affects motor planning skills
Physical and occupational therapists help patients relearn how to move and balance and how to use assistive devices.
Communication, Cognitive and Swallowing Difficulties
A stroke may also affect a patient’s speech, swallowing and cognitive abilities. Effects may include:
- Dysphagia, or difficulty swallowing
- Apraxia of speech affects the ability to form words appropriately
- Aphasia, or the loss of ability to understand or express speech
- Cognitive impairments that include challenges with memory, attention and problem solving.
Speech-language pathologists can help patients with these effects through exercises and technology designed to strengthen swallowing muscles. They can also teach communication techniques to help patients learn to speak, as well as techniques to improve cognition.
Life After Stroke
Download our guide on what to expect after a stroke and how rehabilitation can help you get back to what matters most.
DownloadActivities of Daily Living
After a stroke, you may struggle with completing the activities that make up everyday life, or activities of daily living. Examples of these activities include eating, bathing, dressing or using the bathroom. Occupational therapists can also help you identify activities that are important to you beyond self-care, such as hobbies like gardening or returning to work—and help you practice these tasks and learn new approaches to complete them.
Maximizing Recovery After a Stroke
After a stroke, getting the right rehabilitation can make a substantial difference in your recovery.
According to the 2016 adult stroke rehabilitation guidelines released by the American Heart Association, whenever possible, stroke patients should be treated at an inpatient rehabilitation hospital rather than a skilled nursing facility.
How long it takes to recover after a stroke varies between individuals, but it’s generally believed that the most rapid recovery takes place in the first 90-120 days. After that, continued improvement can be seen for a year or longer.
How Can Rehabilitation Help?
At an inpatient rehabilitation hospital, patients typically receive a minimum of three hours of therapy a day, five days per week. This therapy is a blend of physical, occupational and speech therapy designed to meet your unique needs and improve skills and progresses as a you grow stronger during your stay.
The amount of time spent in therapy means you are able to receive proper repetition of exercises and functional tasks—a key factor in progressing in ability and strength. The advanced technology found in rehabilitation hospitals also helps therapists maximize the benefits of your therapy sessions.
In addition to your therapists, while at inpatient rehabilitation hospitals, you are also seen by rehabilitation physicians and are cared for by registered nurses 24/7 to help manage your medical needs. Other physician specialists will see you as needed, depending on your specific medical conditions. Dietitians, case managers and pharmacists are also members of your interdisciplinary care team.
Your rehabilitation team will work with you and your family to set goals specific to you and your lifestyle prior to your stroke to help you get back to what matters most. Your team will meet weekly to discuss your progress and make any needed adjustments.
At an inpatient rehabilitation hospital, family caregivers are an integral part of your recovery and active participants in your therapy, so you can continue your recovery with them when you leave the hospital. Your rehabilitation team can arrange meetings with family members, and even home visits to help prepare for your transition home.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.



