Diabetes, also known as diabetes mellitus, is a chronic condition that affects more than 37 million Americans, or about 11% of the nation’s total population. According to the CDC, the condition is the seventh leading cause of death, but with proper education, diet and medication, managing diabetes is possible, said Jane Maslonik.
Maslonik is a registered dietitian and certified diabetes educator at Encompass Health Rehabilitation Hospital of Altoona in Pennsylvania. She said about half of her patients at any given time have diabetes.
“I think that really shows the prevalence of this condition,” she said. “Sometimes, we as healthcare providers assume that since they came to us with diabetes that they know how to manage it, but that is not always the case, and things are always changing. If you’ve had diabetes for five to 10 years, it’s still important to stay connected and up-to-date.”
One of the first steps to managing diabetes, Maslonik said, is to understand how diabetes affects your body.
Summary
What is Diabetes?
Simply put, Maslonik said, diabetes impacts the way your body breaks down food for energy. It occurs when glucose, or sugar, builds up in the blood, making it unavailable to use as energy for your body.
When you eat carbohydrates, they are broken down into glucose, which enters your blood stream. If you do not have diabetes, the pancreas senses the rise in blood glucose and, in response to the elevated blood glucose levels, secretes insulin. Insulin unlocks the cells and allows glucose to enter, which lowers your blood glucose levels. Glucose cannot enter the cells without the help of insulin.
If you do not have diabetes, your pancreas and insulin keep your blood glucose levels in an acceptable range. However, if you have diabetes, the pancreas may not make any insulin or enough insulin or there may be a problem with how the body uses the insulin it does make. As a result, the blood glucose levels remain high in the bloodstream causing blood sugar levels to rise. This can lead to complications, which is why managing diabetes properly is so important, Maslonik said.
Types of Diabetes
There are three types of diabetes—Type 1, Type 2 and gestational diabetes. Type 2 is the predominant type of diabetes, making up about 90 to 95% of all diabetes diagnoses, according to the CDC.
“What’s even more alarming is there are so many out there who have Type 2 and don’t even know it,” Maslonik said. “Only about 5% of the population is diagnosed with Type 1. The good news is, there are things you can do to improve with Type 2.”
Type 1
This occurs when the body is producing little to no insulin. This type of diabetes is typically diagnosed during childhood, but in some cases can be diagnosed later in life as well. If you have Type 1 diabetes, you must take daily insulin injections.
Symptoms include:
- Extreme thirst
- Frequent urination
- Increased hunger
- Weight loss
Type 1 diabetes could be hereditary and is thought to be caused by an autoimmune reaction.
Type 2
In Type 2 diabetes, the pancreas isn’t producing enough insulin, or it isn’t using insulin properly. Type 2 diabetes is typically diagnosed after the age of 40 and can be controlled with diet, exercise and oral medications. However, many with Type 2 diabetes may eventually need insulin to control diabetes.
In addition to increased thirst, urination and hunger, symptoms in Type 2 diabetes may also include:
- Fatigue
- Blurry vision
- Dry, itchy skin
- Wounds healing slowly
- Frequent infections
- Numbness or tingling in the feet or hands
Type 2 diabetes is typically caused by a combination of lifestyle and genetic factors such as obesity and race.
Gestational Diabetes
Gestational diabetes happens during pregnancy and occurs when your body can’t make enough insulin during pregnancy. Gestational diabetes typically does not have symptoms but can increase your risk for developing Type 2 diabetes later on.
Early Signs of Diabetes & Diagnosis
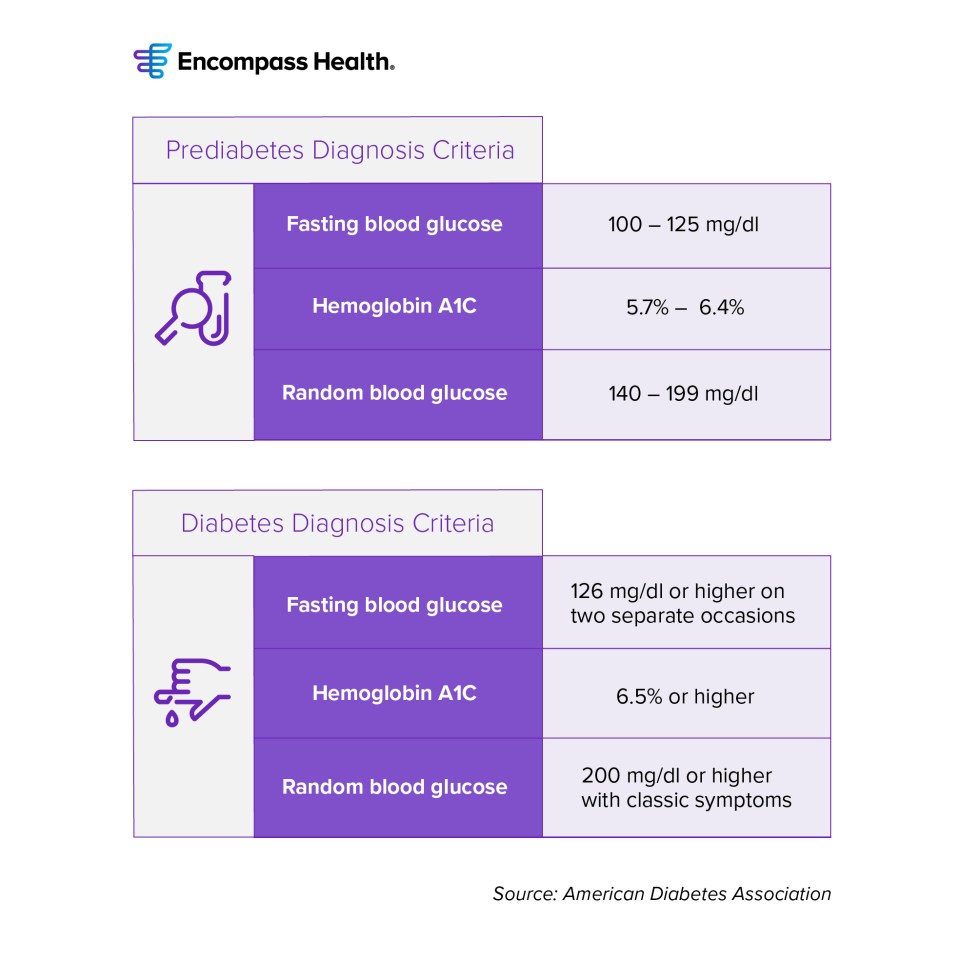
Symptoms of diabetes can come on slowly, and in some cases, there may be no symptoms at all. Before developing Type 2 diabetes, most will have prediabetes. This is a condition where the body is still producing insulin, but blood sugar levels are elevated.
“This is when you really want to take action,” Maslonik said. “When your numbers fall into the pre-diabetic range it means that your pancreas is working harder to keep your blood sugars under control. It’s a good time to start modifying your diet and activity”
A fasting blood glucose level of 99 mg/dl or lower is normal. A fasting blood glucose level of 100 to 125 mg/dl is considered prediabetic. Maslonik said you could still feel fine, but that doesn’t mean you shouldn’t start taking steps to manage your condition. That means adopting a healthier diet and exercise routine, and, in some cases medications. Prediabetes symptoms could include:
- Frequent urination
- Dehydration
- Increased thirst
- Increased hunger
- Unexplained weight loss
- Fatigue
- Dark patches on the skin
Prediabetes is associated with heightened cardiovascular risk. Screening for and treatment of modifiable risk factors for cardiovascular disease is critical if you receive this diagnosis.
According to the American Diabetes Association, you will be diagnosed with diabetes if:
- Your fasting blood glucose levels exceed126 mg/dl or higher on two separate occasions
- Random blood glucose is 200 mg/dl or higher with classic symptoms
- Hemoglobin A1C is 6.5 or higher
Hyperglycemia Vs Hypoglycemia
If you are not managing diabetes properly, you could develop hyperglycemia or hypoglycemia. It is important to know the signs and symptoms of both hyperglycemia and hypoglycemia.
Hyperglycemia is the technical term for high blood sugar and occurs when your body is not producing enough insulin, or it’s not using insulin properly. Over time hyperglycemia, left untreated, can lead to other long-term medical complications. Management of hyperglycemia can include oral medication, insulin, diet and exercise.
There are a variety of factors that could cause you to have hyperglycemia if you have diabetes, including:
- Skipping diabetes medication or not taking the correct amount
- Eating too many carbohydrates
- Stress (physical and emotional)
- Not enough activity or exercise
- Illness/infection
Signs and symptoms of hyperglycemia include:
- Frequent urination
- Thirst
- Tired/weak
- Blurred vision
- Headache
- Dizziness
- Nausea/vomiting
The opposite of hyperglycemia is hypoglycemia, or low blood sugar. A low blood sugar is generally considered a blood glucose less than 70 mg/dl. Hypoglycemia occurs most often due to mismanagement of diabetic medications. It is important to take your medications as prescribed by your doctor to help prevent hypoglycemia and always let your doctor know if you are having any episodes of low blood sugars.
Signs/symptoms of low blood sugar could include:
- Feeling Shaky
- Sleepy
- Numb fingers/limbs
- Sweaty
- Nervousness
- Lightheadedness
- Hunger
- Confused/not thinking clearly
- Headache
- Weakness
Management of hypoglycemia could include consuming carbohydrates, such as juice, gel or a carbohydrate tablet, until your blood level returns to normal, or above 70 mg/dL. If left untreated, hypoglycemia can become a serious medical condition and requirements treatment immediately.
Long-Term Complications from Diabetes
If diabetes is not managed properly over time, Maslonik said, it can lead to other serious and even life-threatening conditions, such as stroke and heart disease.
“There are several complications that can result from years and years of elevated blood sugars,” she said. “Elevated blood sugars circulate through every vessel in your body and over time can cause damage to your organs. The No. 1 killer of people with diabetes is heart disease.”
If you are not managing your diabetes properly, some long-term conditions you could be at risk for include:
Heart disease: According to the CDC, if you have diabetes, you are twice as likely to have heart disease. This risk increases with age. Heart disease includes many conditions related to the heart and blood flow, including stroke.
Chronic kidney disease: Just as high blood sugar levels impact heart over time, they can also impact the kidneys, which could lead to chronic kidney disease. Make sure to have your kidneys checked regularly to help treat and prevent kidney disease.
Nerve damage: Nerve damage is another complication of high blood sugar levels over time. This is referred to as diabetic neuropathy and can cause numbness and pain in your hands, feet and legs. Numbness in your feet can also put you at risk for infection and if untreated lead to amputation due to diabetes. Make sure to perform daily foot checks even if your feet aren’t bothering you, and keep your feet clean and dry. Periodic exams by a podiatrist can prevent complications and reduce the risk of chronic wounds and amputations.
Vision loss: Diabetes can damage your eyes and even lead to vision loss over time. You can have problems with your eyes even if you do not have trouble seeing, so make sure to see your eye doctor regularly.
Free Download: Simple Health Guide
Compiled by expert clinicians, this guide is designed to help you manage your diabetes with simple recipes and tips.
DownloadManaging Diabetes
While there are serious complications and risks that come with the condition, the good news, Maslonik said, is that you can manage your diabetes with medications combined with a healthy lifestyle.
“I like to tell my patients to focus on the positive, the things that they have control over. By focusing on a healthy diet, becoming physically active, and taking medications as prescribed they can manage their blood sugars and help to prevent long term complications,” she said.
Check with your doctor on what the best medications are for you and what tools can help you best manage your diabetes. In most cases, insurance will cover them, Maslonik said.
Aside from medical management of diabetes, Maslonik added that lifestyle is also a key component to control diabetes.
Diet and Nutrition
One of the most important ways to manage your diabetes is by eating the right foods in the right amounts. Learning how to plan appropriate meals and snacks for diabetes, as well as knowing when to eat and how much is very important to managing your blood sugar levels. Follow these healthy eating tips to get started:
- Eat three well-balanced meals daily
- Do not skip meals
- Plan you meals ahead of time
- Eat foods from all food groups
- Choose foods that include whole grains, fresh fruits and vegetables
- Use less fat, sugar and salt
- Cut back on food portions
- Serve food in smaller bowls
- Use luncheon size plates at meals
- Eat more dietary fiber
Exercise
Exercise can also play a big role in managing your diabetes and keeping your blood sugar levels in check. The American Diabetes Association recommends exercising for at least 150 minutes per week. To meet this goal aim to exercise at least 20 minutes a day or 30 minutes five times per week. If you cannot do 30 minutes all at once, Maslonik recommends breaking it up into two or three “mini sessions.” Always begin your activity with a warm up and end with a cool down.
When starting any exercise program it is important to consult with your medical professional to ensure there are no medical issues that would prevent you from safe participation. Once you begin a program, it is important to check your blood sugar before you exercise. If your blood sugar is less than 90 mg/dl, have a snack before you start that contains 15 to 30 grams of complex carbohydrates. If your blood sugar is over 240 mg/dl and you have ketones in your urine, do not exercise. Wait until your blood sugar comes down, and the ketones go away. If your blood sugar is over 300 mg/dl, do not exercise. Lower your blood sugar first.
When exercising for a long period, it is important to check your blood sugar after completion of your workout or during your workout if you are feeling lightheaded or sick. Checking your blood sugar will help you to learn how exercise effects your blood sugar and if your blood sugar has fallen too low. Exercise can have an effect on your blood sugar for up to 12 hours after you completed the activity.
The last piece of advice Maslonik has is to stay informed and learn about advancements in treatments and new options available.
“There are also so many new medicines out there,” she said. “It’s hard to keep up with all the improvements in treatments. When you sit and watch TV, you’re probably going to see a new commercial on products to treat your diabetes. There are a lot of new products out there that make managing diabetes easier. Stay connected, and stay up-to-date.”
About the Expert
Jane Maslonik, MSRD LDN CDCES BC-ADM, is a registered dietitian, certified diabetic care and education specialist and is board certified in advanced diabetic management. She has worked at Encompass Health Altoona for 27 years. For the last eight years, she’s served as the coordinator of the hospital’s Joint Commission Certified Diabetic Program. Maslonik also is an adjunct professor in the nursing program at St Francis University in Loretto, Pennsylvania.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.



