A traumatic brain injury, known as a TBI, is a disruption in the normal function of the brain that can be caused by a blow, bump or jolt to the head, the head suddenly and violently hitting an object, or when an object pierces the skull and enters brain tissue. TBIs are complex and impact each patient differently depending on the level of injury.
In this article
How does TBI Differ from other Brain Injuries?
Dr. Gilbert Siu, who specializes in rehabilitation and is affiliated with Encompass Health Rehabilitation Hospital of Vineland, explained that the difference between traumatic and non-traumatic brain injury is how the injury occurred. “Traumatic brain injury is generally due to external force impacting the brain, such as a car accident, fall, gunshot or concussion, while a non-traumatic brain injury is an internal force affecting the brain,” he said. Examples of non-traumatic brain injury include stroke, infections, COVID-19 and brain cancer.
What Causes TBI?
According to the Centers for Disease Control, the most common causes of TBI are:
- Falls
- Firearm related injuries
- Motor vehicle accidents
Other causes can include sports-related injuries, domestic violence, combat injuries and explosions.
How is TBI Diagnosed?
To diagnose a TBI, clinicians determine the type and severity of the injury. There are several technologies and tools used to evaluate suspected TBI.
Initially clinicians will consider the symptoms and how the injury occurred. A sampling of questions used to make determinations might include:
- How did the injury occur?
- Did the person lose consciousness?
- How long was the person unconscious?
- Did you observe any other changes in alertness, speaking, coordination or other signs of injury?
- Where was the head or other parts of the body struck?
- Can you provide any information about the force of the injury? For example, what hit the person’s head, how far did he or she fall, or was the person thrown from a vehicle?
- Was the person’s body whipped around or severely jarred?
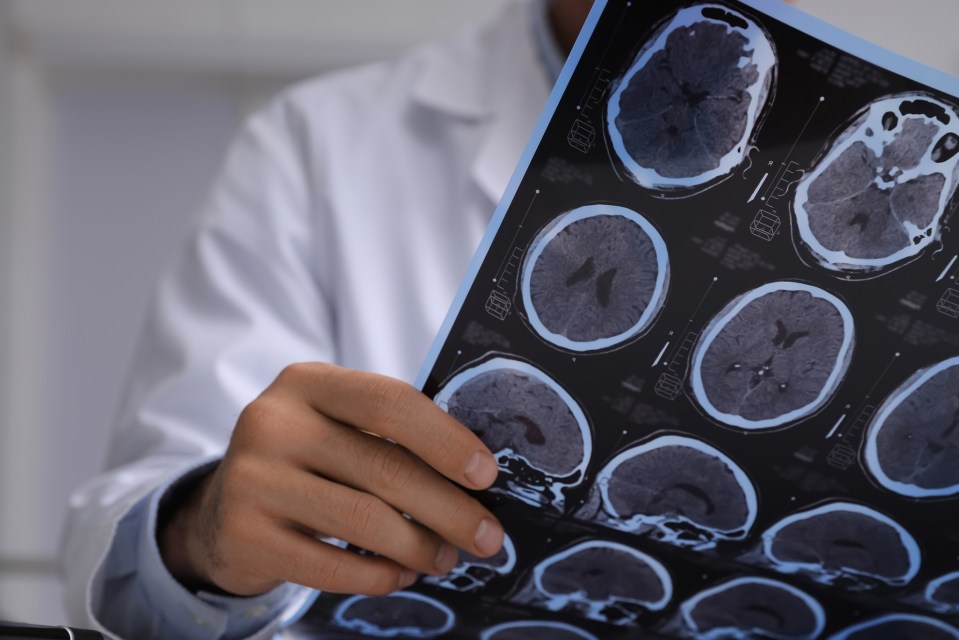
Clinicians also use imaging tests in the case of suspected TBI to take a thorough look at the brain and examine for evidence of brain bleeding (hemorrhage), blood clots, bruised brain tissue and swelling. Those imaging tests could include:
- Computerized tomography (CT) scan: A CT scan uses X-rays to create a detailed view of the brain. A CT scan can quickly visualize fractures and uncover evidence of bleeding in the brain (hemorrhage), blood clots (hematomas), bruised brain tissue (contusions) and brain tissue swelling.
- Magnetic resonance imaging (MRI): An MRI uses radio waves and magnets to create a detailed view of the brain. This test may be used after the person’s condition stabilizes or if symptoms don’t improve soon after the injury.
Clinicians use an assessment called the Glasgow Coma Scale to determine the level of TBI. According to the Brain Injury Institute, the Glasgow Coma Scale is designed to assess the patient’s level of consciousness after brain injury. This scale assigns numbers to eye, verbal and motor responsiveness, then adds those numbers together for a total GCS number between 1 and 15. The lower the number, the more severe the injury.

What are the Levels of TBI?
The level of brain injury falls into three categories:
Mild
- GCS of 13-15 indicates a mild brain injury
- Patients don’t usually lose consciousness and if they do it lasts less than 15 minutes
- Memory loss is temporary; memory returns within 24 hours
- Symptoms resolve within a few days or weeks
- Common form of mild TBI is a concussion
- Medical care isn’t typically needed; however, patients should rest and seek medical attention if symptoms worsen
Moderate:
- GCS score of 9-12
- Unconsciousness lasts for more than 30 minutes, but less than 24 hours
- Diminished ability to communicate
- Partial paralysis
- Loss of cognitive skills
- Memory loss persists for up to a week
- Patients with moderate TBI require immediate medial care to reduce the risk of further damage
Severe:
- GCS of 8 or below
- Unconsciousness persists for six hours or more
- Patients with severe TBI are at a higher risk of long-term complications or fatality and require ongoing medical care
What are the Symptoms of TBI?
“Most common symptoms of TBI depend on the severity of the injury,” Sui said. “For example, a moderate to severe injury will have headaches, muscle weakness, coordination and balance problems, decline in memory and cognition, confusion and agitation. A mild injury commonly presents with dizziness, headaches, fatigue, difficulty concentrating and sensory issues.”
Symptoms of Mild TBI
- Headache
- Confusion
- Lightheadedness
- Dizziness
- Blurred vision
- Ringing in the ears, also known as tinnitus
- Tiredness or sleepiness
- A bad taste in the mouth
- A change in sleep habits
- Behavior or mood changes
- Trouble with memory, concentration, attention or thinking
- Loss of consciousness lasting a few seconds to minutes
- Sensitivity to light or sound
- Nausea or vomiting
Symptoms of Moderate or Severe TBI
Patients with a moderate or severe TBI may experience some of the same symptoms of a mild TBI plus any of the following:
- Headache that gets worse or will not go away
- Loss of vision in one or both eyes
- Repeated vomiting or continued nausea
- Slurred speech
- Convulsions or seizures
- An inability to wake up from sleep
- Enlargement of the pupil (dark center) of one or both eyes
- Numbness or tingling of arms or legs
- Uncoordinated or “clumsy” movements
- Increased confusion, restlessness or agitation
- Loss of consciousness lasting a few minutes to hours
Anybody who suffers a blow to the head should seek medical attention quickly even if symptoms aren’t present. Symptoms might not appear right away so it’s important to be evaluated.
Who is at Risk?
There were 64,000 TBI-related deaths in 2020, according to the CDC, with falls accounting for nearly half of TBI-related hospitalizations. While anyone can experience a TBI, there are certain groups who are at more risk.
- Young children: Adolescents are still developing motor skills and balance. With the brain still developing, children are at a higher risk of long-term affects after TBI.
- People over the age of 65: The risk of falling increases with age resulting in an increased risk of TBI. The CDC reported that about 81% of TBIs in seniors are fall-related. Reducing the risk of fall means reducing risk of TBI.
- Student athletes: Younger athletes between the ages of 15-24 are at a greater risk, particularly if they play contact sports like football, hockey and rugby.
Other groups at greater risk of TBI include:
- Those working in dangerous jobs
- Veterans
- Victims of violence
In addition to at-risk populations, there are groups who are more likely to experience long-term complications due to gaps in healthcare and increased likelihood of additional TBI.
- Racial and ethnic minorities
- Service members and veterans
- People who are experiencing homelessness
- People who are in correctional and detention facilities
- Survivors of domestic violence
- People living in rural areas
What are the Effects of TBI?
The brain is a complex organ that plays a role in nearly every major body system. As the command center, the brain receives information from the five senses (vision, smell, touch, taste and hearing) and sends signals to the body directing the response. It controls thought, memory, emotion, touch, motor skills, vision, breathing, temperature, hunger and other processes. When nerve cells in the brain are damaged, the brain can’t send information in the normal way. This causes changes in abilities and function.
Cognitive Changes (Way of Thinking):
- Short-term memory loss
- Shortened attention span
- Difficulty with problem-solving and following directions
- Partial or complete loss of reading and writing abilities
- Poor judgment
- Communication deficits and loss of vocabulary
- Difficulty learning new things or understanding concepts
Physical Changes:
- Weakness
- Problems with coordination
- Swallowing difficulties
- Changes in the senses (vision, hearing, touch and taste)
- Paralysis and immobility
- Seizures
- Sleep issues
Behavioral/Personality Changes:
- Difficulty with social skills
- Inability to empathize with others
- Tendency to be more self-centered
- Inability to control emotions
- Increases in irritability and frustration
- Inappropriate and/or aggressive behavior, easily angered
- Extreme mood swings
- Depression
Can You Recover from TBI and How Long Does it Take?
Many patients do recover and overcome the challenges associated with TBI. Therapy plays a role in restoring brain function, but patients and caregivers should know that recovery time varies.
“Patients often ask, ‘when can I go back to work?’ and ‘when can I go back to driving?’ I always discuss these questions with the patient and caregivers, so they know returning to these things will be a step-by-step progression,” Dr. Siu said.
It’s difficult to determine an exact timeline for TBI recovery, but typically the first six months after the injury is when the quickest gains are made. During this time, the brain is at a heightened state of plasticity, or healing.

How is TBI Treated in Inpatient Rehabilitation?
Your doctor might recommend inpatient rehabilitation where specialized therapists and doctors develop a plan specific to your needs. In inpatient rehabilitation, registered nurses, many of whom specialize in rehabilitation, are staffed 24/7, and rehabilitation physicians meet with patients at least three times a week. This type of care ensures patients are receiving comprehensive treatment. Patients will undergo three hours of therapy five days per week to re-learn skills they’ll rely on most.
“Our care teams consist of physical therapists, occupational therapists, speech pathologists, case managers, dietitians, pharmacists and neuropsychologists,” Dr. Siu said. There is also an onsite pharmacist to help with medications, and dietitians can assist with special dietary needs. Each patient is also assigned a case manager, who will help prepare them for the next step in their recovery and connect them to resources within their community.
These experts work together for a common goal—restoring the patient’s highest possible level of independence. Therapists working at Encompass Health Rehabilitation Hospital of Braintree shared more about their roles in TBI recovery:
Physical Therapy
Just like the name suggests, physical therapy focuses on restoring patients’ physical capabilities. “This varies depending on the situation and patient, but most goals will be functional,” said Joseph Jameson, a senior physical therapist at Encompass Health Braintree. This includes walking, standing and moving parts of the body. For TBI patients, physical therapy goals include increasing strength, balance, endurance and functionality. Therapy prioritizes safety, both in inpatient rehabilitation and the patient’s home environment. “The plan of treatment is adjusted. We give them strategies to maintain control and evaluate situations to increase safety. It’s important that families are educated and taught how to properly keep a patient safe if they have the inability to make decisions on their own,” Jameson said.
Occupational Therapy
Occupational therapy takes on a more holistic approach, helping patients improve their ability to perform activities of daily living such as dressing, bathing, toileting and grooming. This type of therapy complements progress in physical therapy and can extend beyond basic activities into instrumental activities of daily living such as managing medications, grocery shopping and managing money.
“There are a vast variety of ways a brain injury can affect a patient,” said Ashley Henriksen, an occupational therapist at Encompass Health Braintree. “We base our goals on information given to us about how they were functioning in the community prior to brain injury and the deficits it caused. For example, a patient with a mild TBI who was accustomed to an independent lifestyle before injury would work on upper extremity funtion and learn modified techniques for getting dressed if they experience weakness on one side of their body.” For a more severe TBI, occupational therapists focus on patients’ basic interaction with their environment. “Moderate to severe TBI patients may have deficits in language, cognition, sensation, balance and vision. In those cases, we work on identifying and using functional objects and ADL retraining.”
Speech Therapy
Speech therapy focuses on improving the function of mechanisms above the base of the neck. “From a speech perspective, speech therapists primarily look at speech, language cognition and swallowing for TBI patients,” said Moriah Baker, a speech language pathologist at Encompass Health Braintree. Like other types of therapy, speech therapy is tailored to the patient’s goals and the patient’s previous level of function. Speech therapy can address patients’ ability to speak, understand, read, write, swallow, reason and sustain attention span. “In regards to the activities we do in speech therapy, we try to make them as functional as possible and choose tasks that the patient would have been successful with prior to brain injury,” Baker said.
One of the most common effects of TBI on speech is slurred speech, also known as dysarthria. This speech disorder impacts both the intelligibility and naturalness of speech. To address these deficits, speech therapists use strategies that help with posture, rate (how fast or slow someone talks) and articulation. Other speech therapy activities for TBI patients might include functional math tasks like writing checks or online banking, reading questions, picture/word recall tasks and sequencing tasks (the order of doing certain things.)
Caregivers and TBI
From helping a loved one with daily activities to transporting them to appointments, caregivers often struggle with exhaustion, stress, depression and even anger. When caring for someone recovering from a TBI, it’s important to ask for help and take breaks. In inpatient rehabilitation, case managers prepare patients and their caregivers for discharge and connect them to resources such as:
- Education and tips from the care team on how to help your loved one after discharge
- Home health aides and personal assistants to allow for caregivers to take breaks
- Support groups to connect with others in similar circumstances
- Long-term therapy to help adjust to changes and establish coping skills
- Online resources, books and other materials to educate caregivers
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.