On a daily basis, Patti Esher is keeping a close eye on those around her, looking for signs of infection or sickness.
The COVID-19 pandemic may have made this practice common place. However, Esher has been doing this for years. As a regional infection control preventionist for Encompass Health, she’s charged with not only preventing the spread of the COVID-19 virus, but also any infectious diseases that could spread in the hospital setting.
“We’ve always been tracking and trending data and watching for acquired infections,” Esher said. “We’re always monitoring patients and colleagues, but clearly, it’s been an extremely fast-paced position to be in this last year.”
All inpatient rehabilitation hospitals are required to staff infection control preventionists. However, Encompass Health took that requirement one step further and created infection control protocols specific to the inpatient rehabilitation setting, where unlike in the acute care hospital, patients are spending much of their time outside of their rooms and in a therapy gym or other common areas.
The role of an infection control preventionist pre-pandemic
Esher, who worked as a nurse in the acute care setting for nearly 25 years before transitioning to Encompass Health five years ago, said much of her work as an infection control preventionist revolves around contact tracing, a term all too familiar since COVID-19 was declared a pandemic in March 2020.
Pre-pandemic, though, she was more focused on contagious diseases such as the flu, norovirus and C. difficile—all highly infectious.
“Our No. 1 responsibility is protecting our patients from any healthcare acquired infections,” Esher said. “That’s the goal—to not make any patient sicker and to watch out for our colleagues.”
If an infectious disease is detected in a patient or employee, the infection control preventionist then traces back to where that person has been within the last 72 hours to see who could have been exposed and what precautions need to be taken.
In addition to limiting the spread of infection, the infection preventionist, as the name implies, is also responsible for prevention. That means ensuring patients and employees receive the proper vaccinations. Esher said she also works with other departments, such as environmental services, to ensure hospital rooms and all public spaces are properly cleaned. This became even more important during the pandemic, she added.
The role of an infection control preventionist during a pandemic
Based in Tallahassee, Florida, Esher said her world turned upside down in early April. “That’s when we started really being impacted in our area.”
On the local level, Esher said she and the hospital leadership team were in frequent communication with the state and local health departments. Nationally, she was also working with Encompass Health’s national network of infection control preventionists, as well as the company’s COVID-19 task force, which was in frequent communication with the CDC.
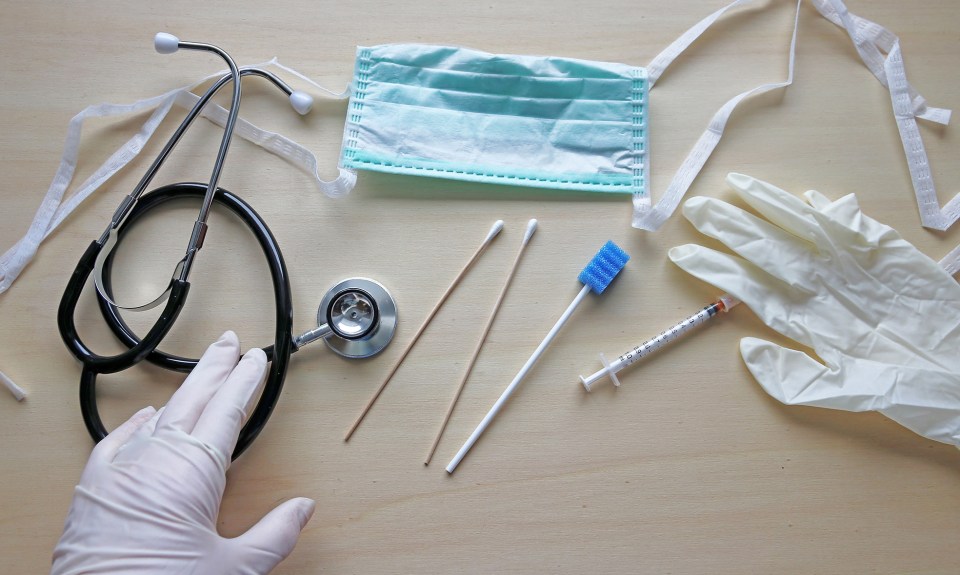
Esher said guidance was constantly changing, and she had to retrain much of the hospital staff, as well as patients, on proper mask wearing and other personal protective equipment.
“It was really good to know we had all these experts there to help us,” Esher said of information coming from the Encompass Health COVID-19 task force, which is made up of clinical leaders as well as operational ones, from supply chain to legal and compliance. “I didn’t feel alone. We were getting daily updates. That was really great to have.”
Those same infection control policies established by Encompass Health more than a decade ago were also effective in handling COVID-positive patients or staff. Therapy could be conducted in the room if needed, and all common areas, such as dayrooms and the cafeteria, were closed.
In order to make use of the gym equipment, they looked to the CDC’s social distancing and masking guidelines and made sure equipment was properly cleaned after each use.
“Really, the true heroes of this were our environmental services department,” Esher said. “They had the responsibility of cleaning the COVID-positive patient rooms, despite their own personal fears.”
Esher worked closely with the department’s employees to ensure they were wearing their PPE properly and that they had a system to air out the rooms that was in keeping with CDC guidance.
A year into the pandemic, they’ve gotten into a routine with COVID infection control protocols. Esher said her newest role is now administering the COVID-19 vaccine, one she couldn’t be more excited about.
“We already completed round two of a vaccination clinic here, and we’ll start a new campaign in the spring,” she said. “We just encourage everyone that, if you can get the vaccine, please consider taking it.”
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.