Healthcare is always evolving, but as clinicians, how do we keep up and implement these changes in a method which is science-based and beneficial to our patients? It’s a challenge most healthcare professionals face, but it can be overcome.
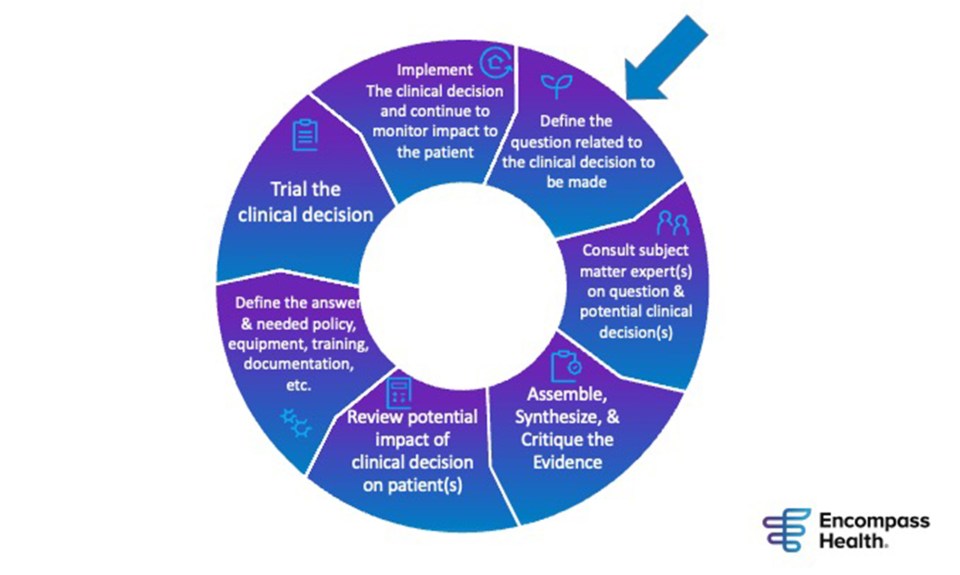
At Encompass Health, our therapy leadership board has developed a method to implement and sustain research into daily practice in our more than 150 rehabilitation hospitals nationwide.
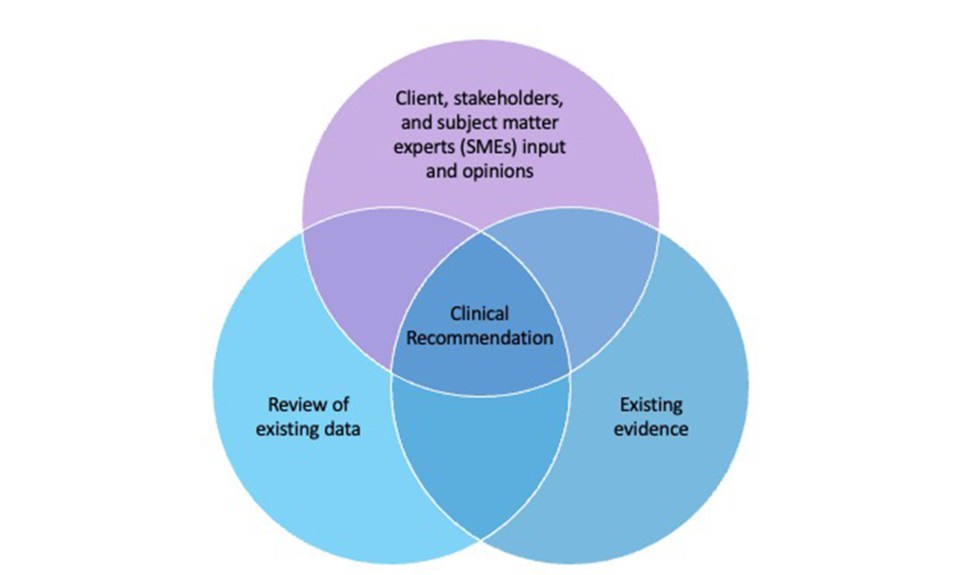
This board is comprised of occupational, speech and physical therapy professionals from across the country. They are responsible for identifying innovative ways to improve care at our hospitals. Looking at published research is just one step in this process we’ve developed. When clinical recommendations to improve care are needed, the board will assemble a team of subject matter experts, analyze the science or evidence and review existing data that may steer clinical decisions and offer an evidence-informed recommendation.
Identifying Gaps in Care
The first thing we do is identify gaps or needs for innovative solutions in clinical practice. For example, take pain management. We were in the middle of the opioid epidemic, and we needed to develop evidence-informed clinical practice guidelines to manage pain in our patient population without opioids. We had a gap in our practice standards there, and there was a need to fill it to improve pain management practices in our hospitals. After identifying this gap we proceeded to implement evidence-informed clinical practice guidelines for acute and chronic pain management utilizing non-pharmacological interventions.
Bringing Subject Matter Experts Together
With the gap identified, we move to assemble all the appropriate clinical experts and stakeholders on the topic and implement evidence-informed clinical practice guidelines. In addition to therapy, experts may include physicians, pharmacists, nurses, dieticians and more, depending on the gap we are trying to address. The subject matter experts’ roles are to review existing data and evidence and use their experience and clinical judgement to recommend and implement appropriate clinical practices. In our example of pain management, we assembled physical, occupational and speech therapy professionals, as well as physicians, nurses and pharmacists to obtain their expertise on best practices to treat pain with non-pharmacological pain management interventions.
Analyzing the Existing Evidence and Data
The next step is to collect and analyze the existing evidence or science and data—both external and internal—and see what it tells us. We search and analyze the evidence for innovative clinical practices that have been proven to produce a positive impact on patient outcomes. And we analyze data for cause-and-effect trends, which may indicate the potential impact of innovative clinical practice on patient outcomes.
When it came to the pain management project, we looked at what the research or evidence said about innovative non-pharmocological pain management interventions. Then, we looked at our data. We analyzed how often we were using opioids versus non-pharmacological interventions. Interventions analyzed included heat and ice, tai chi, yoga, aromatherapy, acupuncture, dry needling and more that we might be able to make better use of in our hospitals.
With all the research and data analyzed, combined with the opinions of our clinical experts, we were then ready to develop and implement innovative clinical practice guidelines.
Piloting and Testing
Before rolling out any new innovative practices or products companywide, we first pilot and test it at one or more of our locations. This provides us valuable feedback from those working directly with patients, so we can make enhancements before implementing the evidence-informed practice companywide.
It also allows us to ensure that clinicians have the needed tools, education and support to properly implement evidence-based practices.
Sustaining the Practices
The process is not complete after companywide implementation. It’s an ongoing effort to keep clinicians trained and educated of evidence-informed innovative practices.
The pain management project took a total of about two years to implement, but when we noticed opioid use in our hospitals start to climb again about six months ago, we regrouped to see how we could reeducate clinicians. A comprehensive training video is now in the works.
Pain management is just one example of how we’re implementing evidence-informed innovative interventions into practice. We used this same methodology to address falls within our hospitals, as well as medication management, to name a few.
One of the hardest things for us as clinicians is implementing research into practice. However, by following this model, we are doing this successfully at Encompass Health, and we are setting the standard for the provision of inpatient rehabilitation services.
Our therapy leadership board is constantly looking for gaps in our services we provide and opportunities to improve patient care and clinical processes, and we typically have four or five of these projects going at a time. This is one of the processes we use to remain innovative at Encompass Health, and most importantly, it’s how we are always improving patient care and outcomes at our hospitals.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.




