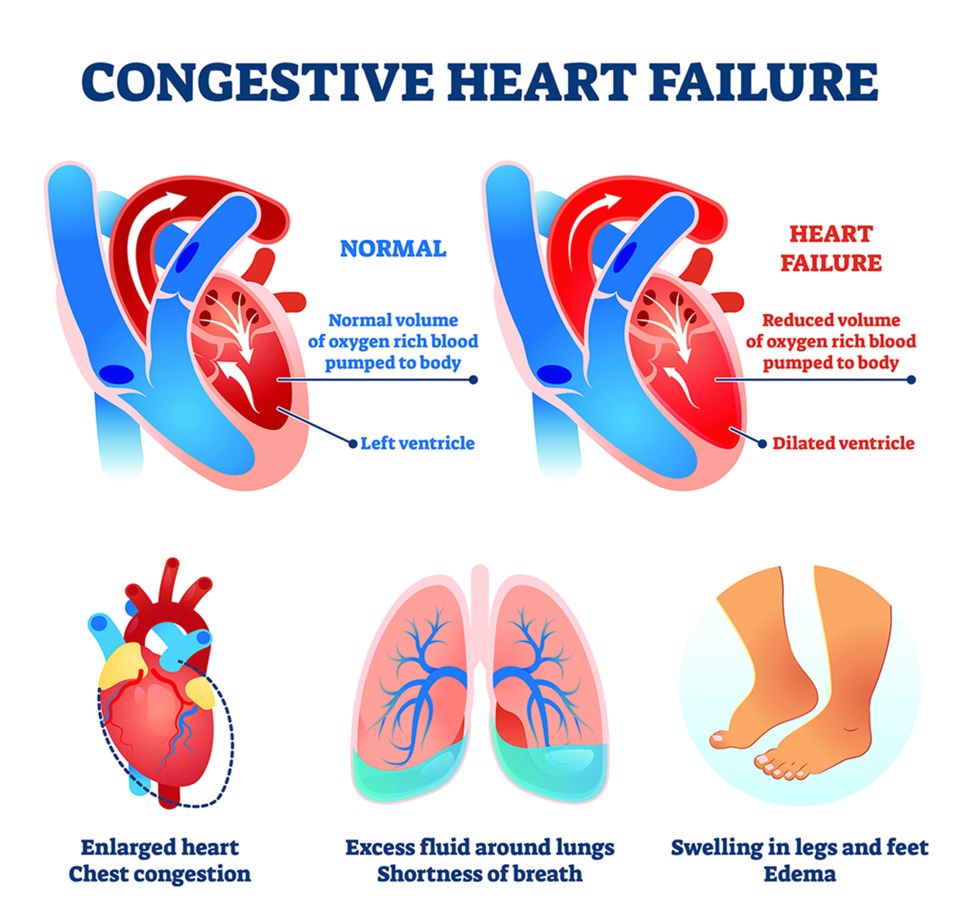
Congestive heart failure (CHF), also sometimes called heart failure, is a condition where the heart does not pump blood efficiently enough to meet the body’s need. Poor contraction of the heart muscle prevents the blood from being efficiently pumped out to other parts of the body. The poor pumping action of the heart means less blood is being pushed out, and blood returning to the heart accumulates, leading to congestion. As a result, fluids build-up in the body, particularly in the ankles, feet and lungs. This risk of kidney failure also increases as fluid and sodium accumulate.
Summary
Causes of Congestive Heart Failure
Many conditions increase the risk of developing heart failure, but the most common cause is coronary artery disease. This occurs when plaque or cholesterol builds up in arteries, causing them to narrow and become stiff. Blood flow through the vessels is decreased, and the risk of heart attack increases. Other conditions linked to CHF include:
- Pulmonary hypertension – increased pressure in the blood moving from the heart to the lungs can lead to congestive heart failure
- Previous heart attack – heart muscle that has been weakened by a heart attack
- High blood pressure – long-term high blood pressure can increase the risk of CHF
- Congenital heart disease – those born with heart defects, vessel malformation and heart valve problems may develop heart failure
- Cardiomyopathy – a disease that damages heart muscle, causing it to thicken, enlarge and stiffen, lessening the heart’s ability to pump
Factors that Increase the Risk of CHF
- High blood levels of cholesterol and fats
- Smoking
- Being overweight
- Diabetes
- Sedentary lifestyle
- High blood pressure
Symptoms of CHF
CHF usually develops slowly over time, but it can also be acute, exhibiting a rapid onset of symptoms. The following symptoms are seen in early CHF:
- Swelling in the ankles and feet
- Shortness of breath
- Fast or irregular heartbeat
- Rapid weight gain
- Wheezing or productive cough
- Weakness or fatigue
- Changes in urination, increase or decrease
According to the American Heart Association, the New York Heart Association Functional Classification is the most commonly used classification system.
- Class I – No symptoms of heart failure with ordinary physical activity
- Class II – Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity produces symptoms such as shortness of breath, heart palpitations and fatigue
- Class III – More severe limitation of physical activity but comfortable at rest. Less than ordinary activity causes fatigue, heart palpitations and shortness of breath
- Class IV – The most severe form of heart failure, symptoms are present even at rest. Unable to perform physical activities without discomfort
Diagnosing Congestive Heart Failure
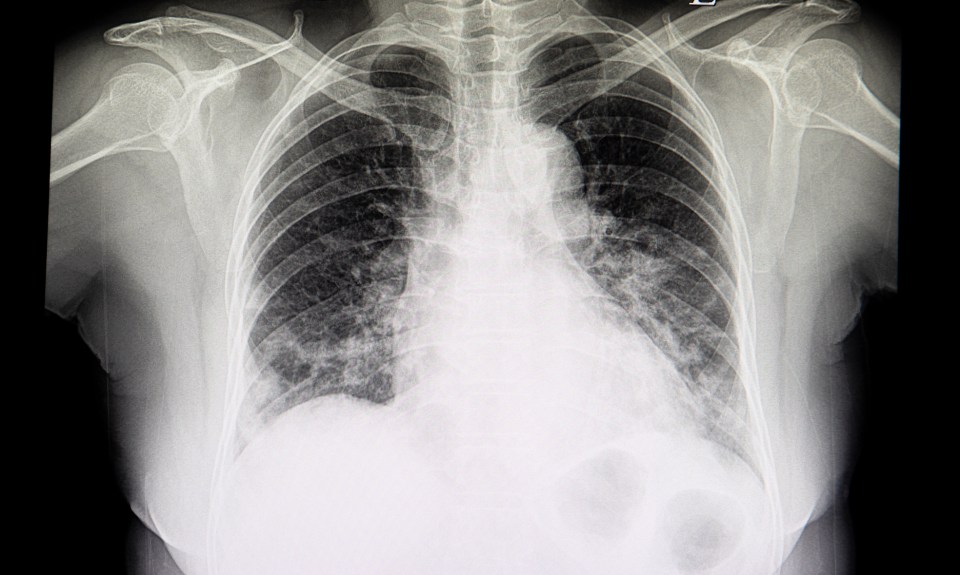
Patients with CHF may have fluid in the lungs or rapid heart rate. Diagnostic testing is needed to provide a firm diagnosis. The medical tests used to diagnose heart failure include:
- Chest X-ray – detects damage to the heart and lungs
- EKG – examines the heart’s electrical activity and can reveal previous heart attack
- Exercise stress test – measures heart activity while on a stationary bike or treadmill or may also be done using a drug that mimics the stress produced by exercise
- Echocardiogram – an ultrasound test that reveals heart structure and function
- Blood tests – can reveal strain on the heart and other organs
- MRI – performed to assess the heart’s structure and blood flow
- Nuclear scans – allows doctors to visualize the heart and blood vessels
- Coronary angiogram – reveals blockages in the heart’s arteries
- Ejection fraction – measures the amount of blood pumped out of the heart each time it beats
Congestive Heart Failure Treatment
There is no cure for CHF, so the goal of treatment is to reduce symptoms, slow the progression of damage to the heart and improve quality of life. Treatment is based on the severity of disease and symptoms.
Lifestyle Changes
Although CHF may be acute, most cases are lifelong and lifestyle changes can be helpful.
- Getting the recommended daily exercise
- Avoiding alcohol and recreational drugs
- Discontinuing the use of tobacco products is recommended
Medications for CHF Treatment
Depending on the specific need and severity of CHF, several medications may be prescribed, including the following:
- ACE inhibitors (angiotensin-converting enzyme) – given to relax blood vessels to lower blood pressure and reduce heart strain
- Vasodilators – used to lessen chest pain and reduce the heart’s oxygen requirement
- Blood thinners – helps prevent blood clots
- Angiotensin receptor blockers – reduces resistance in the blood vessels
- Beta blockers – slows the heart rate and lowers blood pressure
- Diuretics (water pills) – increases urination and pulls fluid away from the heart and lungs
- Digoxin – makes the heart beat stronger and slower and often used in patients with arrythmias
Surgery and Devices for Heart Failure
Some patients may require surgery or implantable devices to treat underlying problems of heart failure. These include:
- Bi-ventricular pacemaker – utilizes three leads, one placed in each the right and left ventricle and a third in the atrium, to coordinate contractions of the heart, allowing the heart to pump more efficiently
- Implantable cardioverter defibrillator (ICD) – the device does not treat CHF but monitors heart rhythm and shocks it back if the rate becomes too fast or the heart stops
- Ventricular assist device (VAD) – usually placed in the left ventricle (but may also be implanted in the right), the device assists the heart in pumping blood to other parts of the body
- Coronary bypass surgery – a blood vessel is taken from the arm, leg or chest and placed in the heart allowing blocked arteries to be bypassed, restoring better blood flow
- Heart valve surgery – damaged valves responsible for heart failure can be repaired or replaced through various procedures, improving heart function
- Heart transplant – in the most severe cases of heart failure, a donor heart may be used as a last resort
Those who have been diagnosed with congestive heart failure should follow a heart-healthy diet, exercise, reduce sodium intake and keep stress to a minimum. It is also important to take all medication as prescribed by a doctor, monitor blood pressure numbers and weigh daily since weight gain could indicate a fluid build-up.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.