The use of dry needling is nothing new. In fact, it’s been around for decades. Today, many physical therapists use it for pain management in the outpatient setting. However, this procedure could also be beneficial to patients with neurological conditions in inpatient rehabilitation.
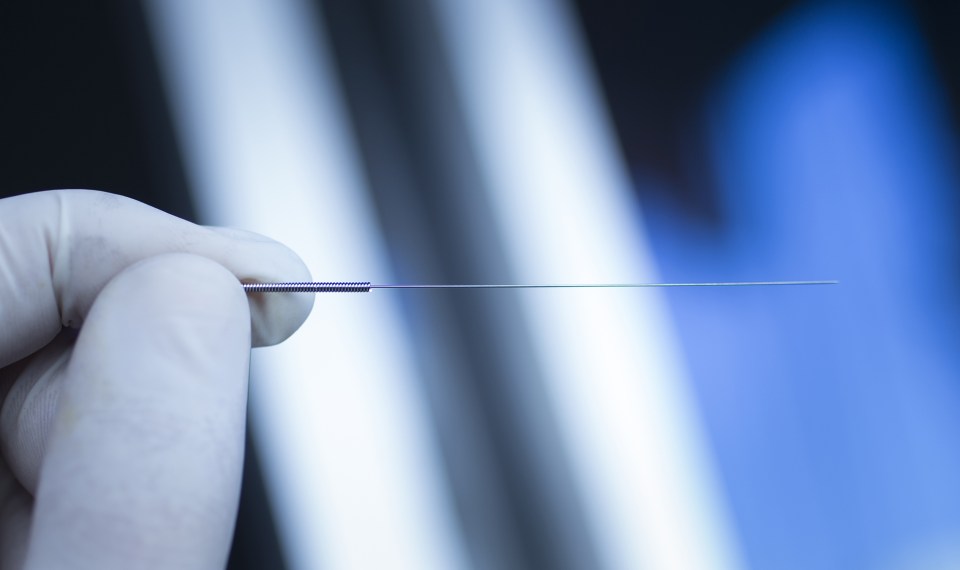
Dry needling, or DN, is a technique that uses small needles to penetrate a “trigger point” in a muscle that is causing pain. After a few sessions, pain can decrease, and more normal muscle function can be restored.
While mostly used to treat orthopedic conditions such as back and joint pain, there is emerging evidence that dry needling could also ease pain and stiffness and restore movement to those with spasticity.
Combining DN with Existing Treatments
Spasticity is the prolonged contraction of a muscle that causes stiffness and limits range of motion. It is a common symptom experienced with a neurological condition such as stroke, traumatic brain injury or multiple sclerosis.
Pain and discomfort resulting from spasticity decreases the quality of life as well as a patient’s ability to function.
Combining existing treatments like physiotherapy, medications and surgery with dry needling could help ease the symptoms of spasticity.
This multimodal approach to treatment can elicit the greatest response, both short- and long-term, making dry needling another beneficial tool in treating this patient population.
An added advantage—in comparison to other treatments, dry needling is cost-effective and has a quick response time.
How Dry Needling Can Help Manage Spasticity
One session of dry needling can produce a hyperalgesic effect, meaning it increases pain pressure thresholds, which leads to a decrease in the pain.
Dry needling also increases blood flow to the affected area. This helps saturate the site with natural opioids and nutrients that aid in healing; it also promotes relaxation.
Single and repeated sessions can create changes at an intracellular level resulting in increased muscle function. Actin and myosin fibers lengthen to decrease the muscle stiffness associated with spasticity. Local twitch responses can also be triggered with dry needling, helping relax the muscle.
These mechanisms likely work together rather than independently to decrease the symptoms of spasticity.
Risks and Challenges for Neurological Conditions
Dry needling can improve muscle stiffness and decrease pain associated with spasticity. This can improve the patient’s ability to perform activities of daily living and their overall quality of life. However, it doesn’t come without risks and challenges.
- Challenges: Cognition can be a barrier to using dry needling with the neuro patient population. Since the skin is punctured, dry needling is considered a medical procedure and requires patient consent, but if their cognition has been impacted by their stroke or other condition, they may not be able to provide consent.
- Risks: The risks are relatively minor, but they do exist. Most patients report soreness that can last for two to three days following a treatment. Bruising can also occur at the site where it is performed, and some patients experience a temporary loss of consciousness or fainting. If the patient is experiencing pain, though, the risks could be worth the relief dry needling can provide almost immediately.
What the Existing Research Reveals
Research on the effectiveness of dry needling for spasticity is limited. However, most existing studies on using this technique for treatment of spasticity showed statistically significant changes in most patients, despite the chronic condition of many of the participants.
Parameters for administration of dry needling also varied from study to study, which could affect the outcomes of these studies. Some studies provided one session of DN, while others provided three to five sessions over the course of a few weeks to months.
Despite the limited research on the use of dry needling for spasticity management, there is evidence to support incorporating dry needling in more settings, including inpatient rehabilitation hospitals.
References
- Bynum R, Garcia O, Herbst E, et al. Effects of Dry Needling on Spasticity and Range of Motion: A Systematic Review. American Journal of Occupational Therapy. 2021;75(1):7501205030p1–7501205030p13. doi:https://doi.org/10.5014/ajot.2021.041798
- Kosem M, Ata E, Yilma F. Does Dry Needling Increase the Efficacy of Botulinum Toxin Injection in the Management of Post-Stroke Spasticity: A Randomized Controlled Study. Archives of Neuropsychiatry. Published online 2021. doi:https://doi.org/10.29399/npa.27733
- Fernández-de-las-Peñas C, Pérez-Bellmunt A, Llurda-Almuzara L, Plaza-Manzano G, De-la-Llave-Rincón AI, Navarro-Santana MJ. Is Dry Needling Effective for the Management of Spasticity, Pain, and Motor Function in Post-Stroke Patients? A Systematic Review and Meta-Analysis. Pain Medicine. 2020;22(1). doi:https://doi.org/10.1093/pm/pnaa392
- del Pilar Pérez-Trujillo M, González-Platas M, Pérez-Martín MY, Revert-Gironés MC, González-Platas J. Dry needling for treating spasticity in multiple sclerosis. Journal of Physical Therapy Science. 2021;33(7):505-510. doi:https://doi.org/10.1589/jpts.33.505
- Sedignhimehr N, Zafarshamspour S, Sadeghi M. Effects of Dry Needling on Muscle Spasticity of the Upper Limb in a Survivor of Traumatic Brain Injjury: A Case Report. Journal of Medical Case Reports. 2022;16(237). Accessed May 22, 2023. https://doi.org/10.1186/s13256-022-03408-5
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.