Welcome to Encompass Health’s 2023 Research Spotlight. In this edition, we will offer a sampling of Encompass Health supported research and publications. As the nation’s largest provider of inpatient rehabilitation, one of our top priorities is to provide our patients with the best experience to help them get back to what matters most. Supporting rehabilitation research and investing in the field of rehabilitation is one way to further this goal.
In This Edition
- Baseline Characteristics and Outcomes for People With and Without COVID-19 Diagnoses Receiving Inpatient Rehabilitation Care
- Metacognitive Strategy Training in Everyday Rehabilitation
- Introducing the 2022 Encompass Health Therapy Grant Recipients
- Tongue Strength Exercising and Swallowing Rehabilitation
- Locomotor and Cognitive Effects of High-Intensity Gait Training in Early Post-Stroke Rehabilitation

Baseline Characteristics and Outcomes for People With and Without COVID-19 Diagnoses Receiving Inpatient Rehabilitation Care
During the pandemic, Encompass Health hospitals were able to provide rehabilitative care to thousands of patients who required inpatient rehabilitation. Drs. Lisa Charbonneau, Joe Stillo, Prateek Grover, Susan McDowell and Jeffery Johns were able to summarize their experience with these patients and demonstrate that they were able to fully participate in, and benefit from the IRF level care.
The research is based on patient data over a 16-month period during the height of the pandemic. It highlights the ability of Encompass Health inpatient rehabilitation hospital care teams to effectively treat patients with the complex medical needs of the COVID-19 population. It showed that COVID recovering patients had similar functional outcomes to patients who did not have COVID.
The results of the study were recently published in the Archives of Rehabilitation Research & Clinical Translation. Read the research paper.
Implementation Science Study: Metacognitive Strategy Training
By Cheryl Miller, DrOT, OTR/L and Elizabeth Skidmore, PhD, OTR/L, FAOTA, FACRM
In 2018, the University of Pittsburgh and Elizabeth Skidmore, PhD were awarded an Encompass Health Therapy Grant to conduct a study at the Encompass Health Rehabilitation Hospital of Sewickley.
The study’s aim was to investigate the feasibility of implementing and embedding metacognitive strategy training into everyday therapy services at our Sewickley hospital, while maintaining fidelity of the intervention.
What is Strategy Training?
Strategy training is a therapy approach that teaches therapists to guide patients through self-discovery while practicing meaningful and salient everyday tasks. Therapists do this while teaching patients self-assessment, self-monitoring and self-initiated problem-solving skills.
In previously published works, patients who received strategy training made comparable functional gains during inpatient rehabilitation, and perhaps most exciting, demonstrated significantly greater functional gains in the months following discharge compared to those who received usual care (Skidmore, et al., 2015).
Strategy training allows therapists to equip their patients with strategy development tools, rather than task-specific skills, to tackle problems they face in the real world.
Strategy Training in Everyday Practice
At Encompass Health Sewickley, Skidmore’s team assessed the impact of strategy training implementation in usual inpatient rehabilitation practice. They observed the delivery of care and outcomes before and after training a therapy team in strategy training (Rebecca Blemler, OT; Gregory Vojcsik, PT; and Amanda Yost, SLP).
The major findings from this initial feasibility study revealed that strategy training implementation was feasible for inpatient rehabilitation, with the team achieving 77% fidelity in real world inpatient practice and maintaining 94% patient satisfaction.
Strategy training implementation was associated with significant changes in practice with a higher frequency of activity-based goals, activity-focused training and guided instructional cues while achieving the same or slightly better functional outcomes.
Comparisons of participants matched on baseline overall GG score, the Center for Medicaid/Medicare’s measurement for functional abilities and goals, and rehabilitation impairment category (n=55) revealed that participants treated with strategy training had greater improvements in overall GG change scores (usual care M=40.49; strategy training M=47.15); difference between groups was greater than the minimal detectable change at 4.7, and a moderate effect size, d=.32).
Participants who received strategy training also had slightly shorter lengths of stay (usual care M=17.11; strategy training M=16.20) and approximately the same rate of community discharge. There was also a statistically significant increase in individual minutes of therapy (usual care M=85.84; strategy training M=93.39, and a statistically significant increase in total minutes (usual care 140.58; strategy training M=148.14).
The outcomes of this study were so promising that Encompass Health continues to work with the University of Pittsburgh and Skidmore to strive to implement this strategy across our network of rehabilitation hospitals. Until this time, strategy training has primarily been studied as an adjunct to usual care, as delivered by specially trained therapists in controlled conditions.
Growing the Study
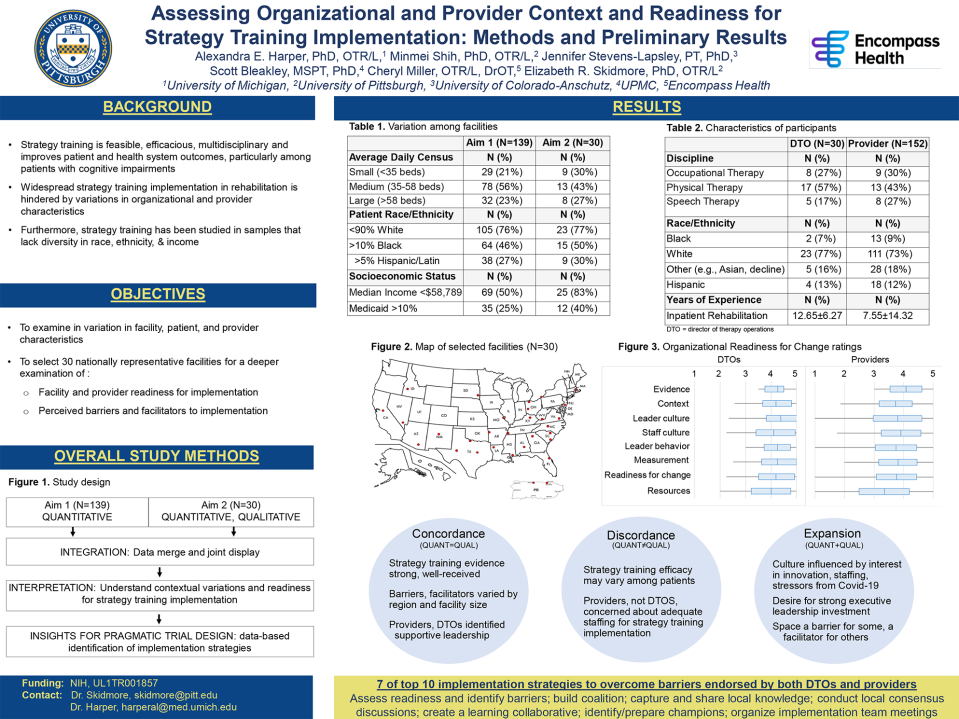
In 2022, Skidmore again partnered with Encompass Health to conduct a study examining the feasibility, acceptability and readiness for strategy training implementation across multiple facilities in preparation for a large-scale pragmatic trial in a sample of 30 Encompass Health inpatient rehabilitation hospitals. The approach leveraged critical partnerships among persons who have received strategy training, academic researchers, rehabilitation providers, directors, corporate leaders and clinical scientists at every phase.
The study team gathered data from 147 Encompass Health hospitals to assess variations in size, clientele and staffing. The study team then selected 30 Encompass Health hospitals that represented variations in geographical location, size (average daily census) and clientele (oversampling facilities that serve a high proportion of marginalized populations based on race, ethnicity, socioeconomic status and payors) to measure readiness for strategy training implementation.
The study team administered standardized questionnaires to examine organizational, director and provider readiness in these 30 facilities. They also conducted focus groups with directors and providers to identify barriers and facilitators to strategy training implementation. Then they created a joint display of quantitative and qualitative data on facility and provider readiness and barriers to strategy training implementation. They learned that the selected facilities have high readiness for strategy training implementation, with consistent support from directors and varied needs identified by providers based on staffing.
This 2022 feasibility study was funded by a National Institute of Health’s Clinical and Translational Science Award.
The findings were presented via poster at the American Congress of Rehabilitation Medicine (ACRM) annual conference in 2022 and are scheduled for a full presentation at the 2023 ACRM annual conference. There is now a plan to apply to the National Institutes of Health National Center for Medical Rehabilitation Research to conduct a pragmatic trial of strategy training implementation in 30 facilities. The team hopes to secure funding to start this trial in 2024.
The first Encompass Health Therapy Grant back in 2018 has facilitated this ongoing research that hopefully will continue in 2024 and beyond. This small grant-funded study in one hospital has the potential to support an ongoing effort to fully implement strategy training in all Encompass Health hospitals.
In doing so, the Encompass Health Therapy Grant program will offer our therapists a new evidence-based therapy approach to care, which leads to improved patient outcomes.
References:
Skidmore ER, Dawson DR, Butters MA, et al. Strategy training shows promise for addressing disability in the first 6 months after stroke. Neurorehabil Neural Repair. 2015;29(7):668-676.
Skidmore ER, Dawson DR, Whyte EM, et al. Developing complex interventions: lessons learned from a pilot study examining strategy training in acute stroke rehabilitation. Clin Rehabil. 2014;28(4):378-387.
Skidmore ER, Whyte EM, Butters MA, Terhorst L, Reynolds CF, 3rd. Strategy training during inpatient rehabilitation may prevent apathy symptoms after acute stroke. PM R. 2015;7(6):562-570.
Sign Up for Research & Resources
Sign up for our newest enewsletter and receive monthly updates from Encompass Health clinical experts on research and resources for healthcare professionals. Just check the box for Resources for Healthcare Professionals.
Subscribe NowEncompass Health 2022 Therapy Grant Award Winners
Encompass Health is excited to announce its 2022 Therapy Grant award recipients. This marked the program’s seventh year, during which time more than 25 research studies have been supported. The 2022 award recipients included:
The Effect of Community Outings on Perception of Preparedness for Home Discharge from an IRF in the Neuro Population Utilizing the B-PREPARED Scale
Encompass Health Rehabilitation Hospital of Sunrise
Principal Investigator: Carrie Keck, OT
The primary purpose of this study is to explore the impact of community outings on patients’ with neurological deficits (stroke, brain injury and spinal cord) perception of preparedness for home discharge from the inpatient rehabilitation setting. Community outings are a recognized treatment intervention for patients in the rehabilitation setting, although review of the literature shows there are limited studies analyzing their impact and even fewer on the impact in the IRF setting. The goal and expected outcome is to prove community outings increase patients’ perception of preparedness for home discharge in the neuro population.
All patients with neuro diagnoses of stroke, brain injury or spinal cord meeting inclusion criteria will complete the B-PREPARED scale on “mark” day (three days before discharge) and receive education on home safety and use of DME for fall prevention. The experimental group will participate in the outing on “ready” day (two days before discharge) with their therapist utilizing non-medical transport and funds provided by the hospital. Patients in both the experimental and control groups will complete a B-PREPARED post scale on their “set” day (the day before discharge). The B-PREPARED scale has been validated as a means to measure patients’ perceptions of their preparedness for hospital discharge home and can be used by clinicians to evaluate discharge interventions.
Early Weight-Bearing Effects on Geriatric Hip Fracture Recovery—A Quantitative Study
University of Missouri
Principal Investigator: Chrissa McClellan
The primary goal of this project is to systematically quantify self-restricted weight bearing and its effects on the physiological and functional outcomes during the early rehabilitation phase of geriatric hip fracture. Our central hypothesis is that self-restricted weight bearing plays a maladaptive role in functional recovery. We propose a prospective, patient-centered study to methodically quantify the weight bearing (via state-of-the-art sensors), the size and quality of a major weight-bearing muscle (via portable musculoskeletal ultrasound), along with clinical evaluations at multiple time points, beginning within seven days post-operative (coinciding with hospitalization post; baseline) and repeating three times during the first 12 weeks after surgery (a time window reflecting outpatient orthopedic follow-up) in 29 patients who underwent internal fixation of hip fracture. The number of steps (as a measure of therapy, via pedometers) will be systematically studied. This study represents an initial proof-of-principle that is feasible for the scope of the present grant mechanism.
Prosthetic Service Deserts Across the United States for Individuals with Amputation
University Enterprises, Inc.
Principal Investigator: Toran D. MacLeod
The purpose of the proposed research is to understand the difference in spatial accessibility to prosthetic services in post-acute care rehabilitation across the United States for those at risk of limb loss and how this affects clinical outcomes. This will be done by comparing prosthetist business locations to measures of need for their services (prevalence of individuals at risk for amputation as measured by prevalence of diagnosed diabetes and obesity). This analysis will result in maps showing the spatial distribution of areas with high and low patient to available prosthetic service provider ratios, highlighting areas with greater current and future need for provision of prosthetic services. We will also evaluate if there is a relationship between patient to provider ratios and patient quality of rehabilitative care. Results from this study can be applied to improve the quality of care for those needing prosthetic services with the goal of easing access to quality care.

Tongue Strengthening Exercise Methods During Swallowing Rehabilitation
Sarah H. Szynkiewicz, Ph.D. CCC/SLP
Assistant Professor
Communication Sciences and Disorders
Encompass Health has funded a multi-site, randomized controlled trial aimed at comparing tongue strength exercises in healthy, community-dwelling adults. The study, Determining an Optimal Delivery Method for Tongue Strengthening During Swallowing Rehabilitation: Building a Framework for Clinical Practice, compares tongue strength outcomes for maximum (push as hard as you can) vs. progressive (gradually increasing intensity at a percentage of maximum) effort exercises, as well as visual biofeedback with a device vs. no visuals while completing the exercises three times a week for eight weeks.
The Study
More than 80 participants were randomly assigned to one of four treatment groups:
- Tongue resistance exercises completed at maximum intensity with no visual biofeedback
- Tongue resistance exercises completed at progressive intensity with no visual biofeedback
- Tongue resistance exercises completed at maximum intensity with visual biofeedback
- Tongue resistance exercises completed at progressive intensity with visual biofeedback
Exercise adherence data was collected throughout the study. After eight weeks of the exercise program, half of the participants continued with an exercise maintenance program, and their tongue strength was compared to those who did not complete the maintenance program one month later.
The Results
After eight weeks of tongue exercise at home, participants demonstrated improved tongue strength across all tasks, regardless of intensity or visual biofeedback.
For the groups who had visual biofeedback with the device, completing the maximum intensity task made accuracy easier to achieve during home practice compared to the progressive intensity task.
All four treatment groups had the same levels of adherence. Adherence and accuracy levels did not change as participants progressed through the study, and neither one was correlated with tongue strength gains.
All treatment groups maintained strength gains at a one-month follow-up for all tasks; completing a maintenance program did not affect strength at the follow-up visit compared to those who did not complete maintenance.
In summary, the data suggest the opportunity for flexibility in designing tongue strengthening exercise protocols—that the protocol can be designed to fit the individual needs of each patient.
Lindsay Griffin, Ph.D, CCC-SLP, Rachel Mulheren, Ph.D, CCC-SLP, Erin Kamarunas, Ph.D, CCC-SLP, Teresa Drulia, Ph.D, CCC-SLP, Kelsey Murray, MS, CCC-SLP, Theresa Lee, & Sarah Szynkiewicz, Ph.D, CCC-SLP
Locomotor and Cognitive Effects of High-Intensity Gait Training in Early Post-Stroke Rehabilitation
By Jason Karstens, PT
Encompass Health Rehabilitation Hospital of East Valley
Around 30% of individuals who have a stroke will have cognitive deficits.1 Research suggests that some physical therapy interventions may cause generalized neuroplastic changes to the brain post-stroke.2,3 These changes, linked to intensity of training, can prime the brain to improve motor learning, among other benefits.4
High intensity gait training (HIGT) is one intervention that has been shown to be feasible and beneficial from a locomotor recovery standpoint.5 There is currently a lack of research on how these interventions may affect both cognition and locomotor function, especially in the acute phase of recovery. The purpose of this study is to determine if locomotor and cognitive function can be improved in individuals in the acute phase of stroke rehabilitation with high intensity gait training compared to usual care.
Participants
Individuals in the acute phase of stroke rehabilitation (<3 months post stroke) currently in inpatient rehabilitation, who require speech therapy services, have no history of previous stroke or COVID and have been medically cleared by a physician to participate in high intensity cardiovascular training.
Methods
A randomized controlled trial was used to compare cognitive and locomotor outcomes in usual care (n=10) versus high intensity gait training (n=10) in patients in the acute phase of recovery (<3 months post). Outcomes included total motor score as measured by the inpatient rehabilitation facility patient assessment instrument (IRF-PAI), the Montreal cognitive assessment (MoCA) and Expression of Ideas and Wants and Understanding of Verbal Content as measured by the IRF-PAI. A generalized estimating equations (GEE) approach was used to account for multiple measurements from patients.
Results
Both the usual care group and HIGT group made statistically significant improvements in motor scores, MoCA scores and Expression of Ideas and Wants (p<0.05). There was no significant difference in improvements between groups in motor scores or the MoCA. Changes in Expression of Ideas and Wants were significantly greater in the HIGT group compared to the usual care group (p<0.05).
Conclusions
HIGT is as effective as usual care in improving locomotor and cognitive outcomes in acute stroke rehabilitation despite the HIGT group having significantly lower motor and cognitive scores at baseline. No adverse events occurred in either group, contributing to previous findings that HIGT is as safe as usual care in acute stroke rehabilitation. Further studies are recommended to identify alternative cognitive assessments and subgroups within the stroke population (cortical vs subcortical, laterality of lesion, etc.) that may respond differently to the intervention. Continued consideration of various measurements of intensity of HIGT are recommended as well due to medication limitations in heart rate elevation in the acute stroke population.
Clinical Implications
HIGT is safe and as effective in improving locomotor function compared to usual care in the acute phase of stroke rehabilitation. There may be secondary benefits of improving cognition.
References
Kalaria, R. N., Akinyemi, R., & Ihara, M. (2016). Stroke injury, cognitive impairment and vascular dementia. https://doi.org/10.1016/j.bbadis.2016.01.015
Li, X., Charalambous, C. C., Reisman, D. S., & Morton, S. M. (2019). A Short Bout of High-intensity Exercise Alters Ipsilesional Motor Cortical Excitability Post-stroke. https://doi.org/10.1080/10749357.2019.1623458
Penna, L. G., Pinheiro, J. P., Ramalho, S. H. R., & Ribeiro, C. F. (2021). Effects of aerobic physical exercise on neuroplasticity after stroke: Systematic review. In Arquivos de Neuro-Psiquiatria (Vol. 79, Issue 9, pp. 832–843). Associacao Arquivos de Neuro-Psiquiatria. https://doi.org/10.1590/0004-282X-ANP-2020-0551
Moriarty, T. A., Mermier, C., Kravitz, L., Gibson, A., Beltz, N., & Zuhl, M. (2019). Acute Aerobic Exercise Based Cognitive and Motor Priming: Practical Applications and Mechanisms. Frontiers in Psychology, 10. https://doi.org/10.3389/fpsyg.2019.02790
Moore, J. L., Nordvik, J. E., Erichsen, A., Rosseland, I., Bø, E., & Hornby, T. G. (2020). Implementation of High-Intensity Stepping Training during Inpatient Stroke Rehabilitation Improves Functional Outcomes. Stroke, 563–570. https://doi.org/10.1161/STROKEAHA.119.027450
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.



