We’ve all been there: That moment at the end of a clinical visit when you’re handed a list of medications and instructed to head to your local pharmacy—with no other advice. Upon review of the Rx list, the questions roll in. “How do I pronounce this?” “Do I need to take these pills with food?” “What should I do if I miss a dose?”
Some research suggests that medication misuse ranks as a leading cause of death in the United States. While medication errors aren’t always fatal, they can still cause serious complications for people living with chronic illness or recovering from an injury. According to MedActionPlan, only one third of patients follow Rx instructions as prescribed. Another third take their medications improperly or not at all.
Medication errors often stem from misunderstanding the dose, frequency or nutrition requirements advised for a specific drug. Poor communication during care transitions can put elderly patients, especially those with complex medication regimens, at risk for medication errors.
“From a rehabilitation standpoint, these errors can seriously impede a patient’s recovery and can even contribute to disease progression,” said Shawn Myers, national director of pharmacy for Encompass Health. “Non-adherence is a major factor in making a patient a candidate for hospital readmission.”
How Encompass Health Is Improving Patient Rx Education
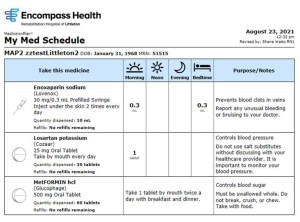
In early October, Encompass Health hospitals began using an upgraded medication discharge tool. Unlike medication lists of the past, the MedActionPlan® tool integrates with the Electronic Medical Records (EMR) system to generate a visual overview of the medication discharge plan using pictures and easy-to-read charts.
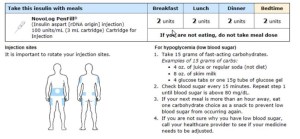
The print-out shows patients when medications should be taken (morning, noon or night) alongside an image depicting the type of drug (tablet, drop, inhaler or injection) and the dose. A short descriptor explains what the drug does and includes guidelines for how it should be taken. To improve accessibility, the tool can also print medication lists in large font sizes and in the patient’s preferred language.
“It’s better than a standard, text-heavy medication schedule; it’s an action plan presented in terms that are clear and easy to understand,” Myers said.
Detailed action plans for diabetes—a particularly high-risk disease that comes with complicated medication regimes—can help ensure patients know when to take their insulin, where injections should be administered and the required insulin-to-carb ratio. Anticoagulants (blood thinners) are another class of medications that require strict adherence. Anticoagulation action plans combine a visual weekly schedule with specific dietary guidelines.
While this tool is new for most Encompass Health hospitals, Myers and his team expect to see improved patient outcomes very quickly. They will use data to track the effectiveness of the new tool by reviewing Encompass Health’s patient satisfaction scores over time, particularly on the routine question, “How well do you feel your medications were explained to you?”
Extra Steps You Can Take to Prevent Medication Mistakes
Health literacy—in essence, the ability to understand and act on medical advice—can be an obstacle to medication adherence. Other social determinants of health can also play a role. Asking family members, trusted neighbors, caregivers or home health aides to help with your medication regime is a great way to create accountability and keep you on track.
Other health factors such as vision and memory loss can contribute to medication misuse. If a caregiver is not available to help you with medications, tools such as pill boxes, automated timers and automatic pill dispensers can help ensure you take the right medications at the right time each day.
Above all, it’s important to have clear medication instructions when you leave the clinic or hospital. It’s especially important to understand which supplements, foods and medications can be toxic when mixed. If you have unanswered questions about the medications being prescribed to you, don’t be afraid to ask your physician or care team for simplified instructions.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.



