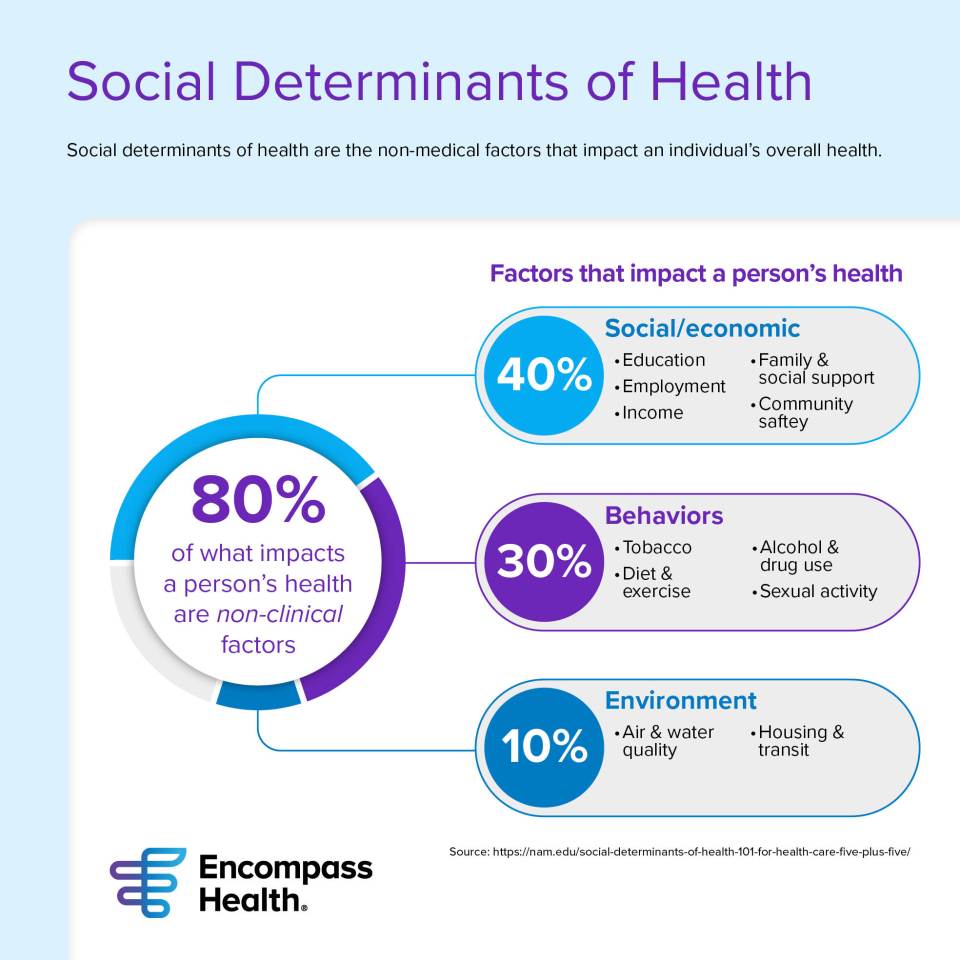
After a patient leaves the hospital, there are several factors that could elevate their risk of a hospital readmission. You may be surprised to learn that the cause of a readmission may not be related to a patient’s medical condition. Social determinants of health are the non-medical factors that influence a person’s overall health. They include anything from access to healthy food to employment and education level.
“A large part of what impacts a person’s health is not clinical; it’s more behavioral, cultural or environmental,” said Dina Walker, national director of case management for Encompass Health. “Factors impacting health could be level of education, economic means, lifestyle and the area in which a patient lives. For example, if a patient has a low educational level and/or has a limited understanding of medical or clinical information, their health may be negatively impacted. If they live in a rural setting, they may not have convenient access to receive care from physician practices, specialists or urgent care centers.”
These same factors also play a role in the likelihood of a patient readmitting to the hospital.
As part of Encompass Health’s ongoing efforts to reduce hospital readmissions, the company developed a social determinants of health risk assessment specific to patients leaving the inpatient rehabilitation setting. The assessment is part of the company’s overall Readmission Prevention Program, which combines clinical and nonclinical factors to determine the risk of a hospital readmission after a patient leaves an Encompass Health rehabilitation hospital.
The proper assessment for the proper patient
A social determinant of health risk assessment is typically presented to a patient before they discharge from the hospital setting. It’s a list of questions that assesses any social or economic barriers that could impact the patient’s health.
Before developing a new risk assessment, Walker said they examined existing standard assessments such as PRAPARE or WellRx, for example.
“Basically, what’s out there is geared toward the acute hospital or population health management, where they are managing a group of patients for months—neither of those models fit inpatient rehab,” she said. “Our patients are with us for about two weeks, they discharge, and we may follow them telephonically a few days after that.”
Most of the existing assessments ask questions with the single goal of collecting data. The other tools may help to assess social barriers that influence a patient’s health, but they offer no solutions or interventions to help the patient. “In designing our tool, we wanted to take that next step,” Walker added. “We want to help these patients. We want to offer interventions and maybe avoid a readmission while we’re at it.”
Walker added that they wanted the assessment to be relevant to Encompass Health’s patient population, which is predominantly older adults with the average patient at 74 years old. Questions on the assessment are directed toward that population.
Assessments plus action
When developing the assessment, Walker wanted to keep it simple, but more importantly, she wanted to make it meaningful.
“We wanted the questions to be easy for the patient to understand and to answer, so we are building simple questions that can be answered with a Yes or No response”, she said.
For example, one question addresses the patient’s access to care in their area. If they live an hour or more away from a medical facility, the case manager can then explore the possibility of telemedicine for the patient. Another question addresses their ability to pay their utilities, a possible indicator of low income. If one or more of their utilities have been shut off recently, the case manager can then connect the patient with local utility assistance, churches or other charitable organizations.
The assessment is limited to six questions, and case managers enter answers into the company’s electronic medical record system. The yes or positive responses to the assessment questions can then be learned by the readmission risk model and used to help predict the probability of a patient’s overall readmission risk as part of Encompass Health’s Readmission Prevention Program. If the patient has a high risk score, the case manager will continue to connect with them after discharge, communicate with the patient’s primary care physician and home health provider and take necessary steps to prevent a hospital readmission.
What’s next?
The Readmission Prevention Program uses a predictive algorithm that was developed from Encompass Health’s inpatient rehabilitation electronic medical records. The model is always changing and learning and was previously only using clinical variables to determine a patient’s risk of a hospital readmission. With information collected from the social determinants of health assessment, a readmission risk score is more accurate and meaningful, and the discharge plan is created with the whole patient in mind.
The new social determinants assessment will also help case managers get ahead of future CMS requirements that will most likely include mandatory social determinants of health questions during the discharge planning.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.



