Encompass Health was again a proud sponsor of ARN REACH 2019, an annual national gathering of rehabilitation nurses, which wrapped up on Nov. 9. In addition to sponsoring the keynote speaker, 25 Encompass Health employees presented posters on varying clinical topics, and three employees presented on best practices implemented at Encompass Health rehabilitation hospitals. Learn more about their topics below.
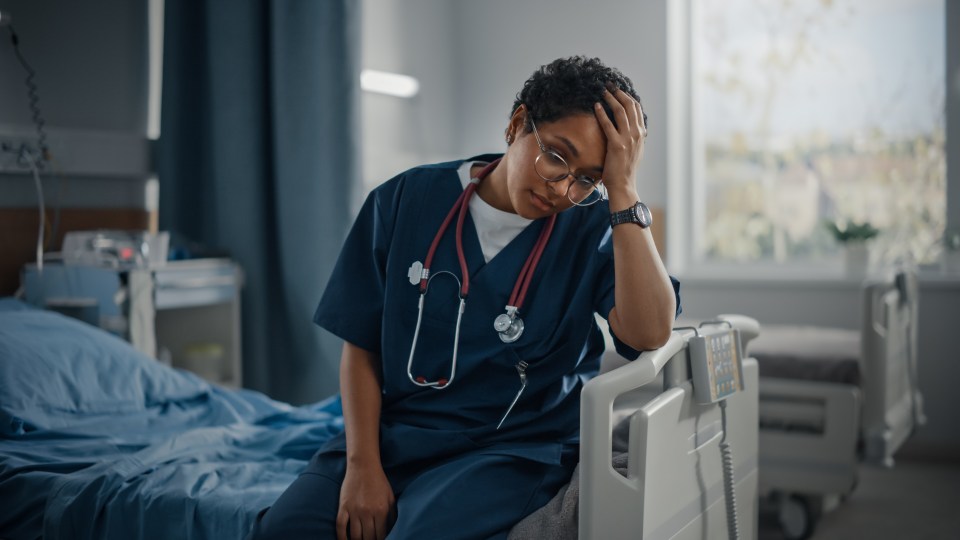
“Fostering a Healthy Work Environment for Nurses”

Coleen Rossi, MBA, RN, CCM, CRRN, chief nursing officer
Encompass Health Rehabilitation Hospital of Toms River
Born out of recognition that a healthy work environment could improve attitudes and engagement of both experienced and novice nurses, the nursing staffing council at Encompass Health Rehabilitation Hospital of Toms River was created. The staffing council is a group of Encompass Health employees who voluntarily participate in monthly meetings and attend educational sessions hosted by the Organization of Nurse Leaders of New Jersey (ONL-NJ). Led by the hospital’s CNO, more than half of the council members are bedside nurses. As the first inpatient rehabilitation hospital in New Jersey to participate in the ONL-NJ healthy work environment program, the council has delivered early dividends.
The program’s educational topics include skilled communication, effective decision making, authentic leadership, appropriate staffing and meaningful recognition. While the group began with a strong desire to analyze and rework the staffing matrix, group discussions have centered around personal development, filling knowledge gaps, improving understanding of hospital operations, fostering adherence to meal and break schedules, and a strong desire to work to the top of professional license. Regular access to the CNO has provided momentum to eliminate barriers to efficient care through collaboration with supporting departments. This collaboration has increased staff communication and improved care at the bedside.
“Palliative Care in Rehabilitation”

Natasha Poorman, BSN, CRRN, infection preventionist
Encompass Health Rehabilitation Hospital of Nittany Valley
Palliative care is an overall approach to care that can alleviate suffering for those living with serious illness, regardless of prognosis. Given the growing prevalence of heart failure, with an estimated 5.9 million adults in the United States currently carrying the diagnosis, increasing comfort and improving a person’s quality of life is key to compassionate care. For this reason, Encompass Health Rehabilitation Hospital of Nittany Valley in Pennsylvania has incorporated a palliative care screening tool into the routine assessment of all heart failure patients in their hospital.
Performed within the first three days of admission, the interdisciplinary team uses the screening tool to recognize patients with palliative care needs and request a referral to their palliative care physician. Adding the palliative care screening tool to their heart failure program has led to an increase in awareness and education of this type of care management in patients, caregivers and staff. Because of this awareness, the Encompass Health Nittany Valley team feels they are better able to identify patients with a crucial need for a potential increase in treatment, follow-up and support post discharge. Poorman believes that palliative care is a positive addition to any heart failure management program.
“UrINe-VITED Bladder Program”

Carissa Augustyn, MSN, RN, CRRN, director of quality and risk management
Yuma Rehabilitation Hospital, a partnership of Encompass Health & Yuma Regional Medical Center
In early 2018, the interdisciplinary team at Yuma Rehabilitation Hospital in Arizona reviewed the new Evidence Based Practice Guidelines (EBP) and chose to pay special attention to the bladder aspect with the goal of piloting a bladder management program to their stroke population. The team created tools to make the EBP practical and applicable to the frontline nurse, consulting EBP author Christine Cave throughout the process, even tasking Cave with approving all worksheets used in the new program.
The new process includes a focused admission assessment, 72 hour assessment period, patient education, toileting, urge suppression and pelvic floor exercises. The hospital’s physical therapists, occupational therapists, speech language pathologists and registered nurses were trained in preparation for the process change. Since the implementation of the UrINe-VITED program, the hospital has seen an increase in patients who are continent on discharge, as well as a two point increase in bladder function change. The management team has also seen increased staff and patient engagement with the program since its launch.
The content of this site is for informational purposes only and should not be taken as professional medical advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding any medical conditions or treatments.